Understanding the Diabetes Honeymoon Period
The “honeymoon period” in diabetes, particularly in Type 1 diabetes, is a phase that often follows the initial diagnosis and treatment. During this time, the body still produces some insulin, leading to a temporary reduction in the need for insulin injections or other medications. It’s a hopeful phase, as blood sugar levels are easier to manage and the overall impact of diabetes seems less severe. However, understanding this period and how to navigate it is crucial for long-term diabetes management and overall health. The duration and intensity of the honeymoon period vary significantly from person to person, making it important to be aware of its characteristics and potential challenges. This article unveils the top 5 secrets to prolonging this phase and managing diabetes effectively.
What is the Honeymoon Period?
The honeymoon period is a transient phase that occurs after the onset of Type 1 diabetes, and sometimes in newly diagnosed Type 2 patients, where the pancreas continues to produce some insulin. This residual insulin production allows for better blood sugar control, often resulting in lower insulin dosages and fewer episodes of hyperglycemia or hypoglycemia. This period can last from a few weeks to several months, or even up to a year or more in some cases. During this time, patients may experience improved energy levels and reduced symptoms of diabetes. However, it’s essential to recognize that this is not a cure, and eventually, the body’s insulin production will diminish further, requiring adjustments in treatment.
The Science Behind the Honeymoon

The honeymoon period is a result of the interplay between the body’s immune system, the remaining beta cells in the pancreas, and the introduction of insulin therapy. When type 1 diabetes is first diagnosed, the immune system is actively attacking the insulin-producing beta cells. However, some beta cells may survive the initial autoimmune attack. When insulin therapy is initiated, it provides the body with the insulin it needs, reducing the stress on the remaining beta cells. This reduced stress allows the beta cells to function more effectively, leading to increased insulin production. The duration of the honeymoon depends on how many beta cells remain and how well the autoimmune attack is managed. This phase is characterized by fluctuating insulin needs and a delicate balance between treatment and lifestyle.
Factors Influencing the Honeymoon Period
Several factors can influence the duration and intensity of the diabetes honeymoon period. Early and aggressive insulin therapy can help preserve beta cell function, potentially extending the honeymoon. The individual’s immune response and the extent of beta cell destruction at the time of diagnosis also play a significant role. Moreover, lifestyle factors, such as diet and exercise, can impact the body’s response to insulin and blood sugar control. Genetic predisposition and age at diagnosis can also affect the duration of the honeymoon phase. Careful management of these factors through a combination of medical interventions and lifestyle adjustments can help maximize the benefits of the honeymoon period and improve long-term outcomes.
Top 5 Secrets to Prolonging the Diabetes Honeymoon
Early Diagnosis and Treatment
Early detection of diabetes and the immediate initiation of treatment are crucial in preserving beta cell function and potentially extending the honeymoon period. Prompt diagnosis allows for early intervention, often minimizing the damage to the beta cells from the autoimmune response. This can be achieved by recognizing the early signs of diabetes, such as increased thirst, frequent urination, unexplained weight loss, and fatigue. Regular blood sugar testing, especially if there is a family history of diabetes, is a good way to catch it early. When diagnosed early, insulin therapy or other treatments can be started promptly, helping to protect the remaining beta cells and prolong the honeymoon phase.
Intensive Insulin Therapy
Intensive insulin therapy is another key strategy in prolonging the diabetes honeymoon. This approach involves multiple daily insulin injections or the use of an insulin pump to mimic the body’s natural insulin release patterns. By closely managing blood sugar levels, intensive insulin therapy reduces the stress on the remaining beta cells, helping to preserve their function. This strategy may involve frequent blood sugar monitoring to make necessary adjustments to insulin dosages. Working closely with a healthcare team to develop an individualized insulin regimen is essential. The goal is to keep blood glucose levels within a target range, which will help in maintaining the function of the beta cells and extending the honeymoon period.
Lifestyle Modifications
Lifestyle adjustments are an integral part of diabetes management and play a significant role in extending the honeymoon period. Making changes in your daily habits, such as adopting a healthy diet and engaging in regular physical activity, can significantly impact the duration of the honeymoon and improve overall health. These lifestyle changes can improve insulin sensitivity, help regulate blood sugar levels, and support weight management, all of which are beneficial for diabetes management. Lifestyle modifications are not only important during the honeymoon period but also for long-term health.
Dietary Adjustments
A well-balanced diet is essential for managing blood sugar levels and extending the honeymoon period. Focus on consuming whole foods, including fruits, vegetables, lean proteins, and whole grains. Limit your intake of processed foods, sugary drinks, and saturated and trans fats. A registered dietitian can help you create a personalized meal plan that considers your individual needs and preferences. The goal is to manage carbohydrate intake, choose foods with a low glycemic index, and maintain consistent meal times. This dietary approach helps keep blood sugar levels stable, supporting the function of the remaining beta cells.
Regular Exercise
Regular physical activity can significantly improve insulin sensitivity and help regulate blood sugar levels. Exercise allows the muscles to utilize glucose more effectively, which helps lower blood sugar. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, combined with strength training exercises at least twice a week. Before beginning any exercise program, consult your doctor to ensure it is safe. Monitor blood sugar levels before, during, and after exercise to understand how your body responds. Staying active is one of the best ways to maintain blood sugar control during the honeymoon period.
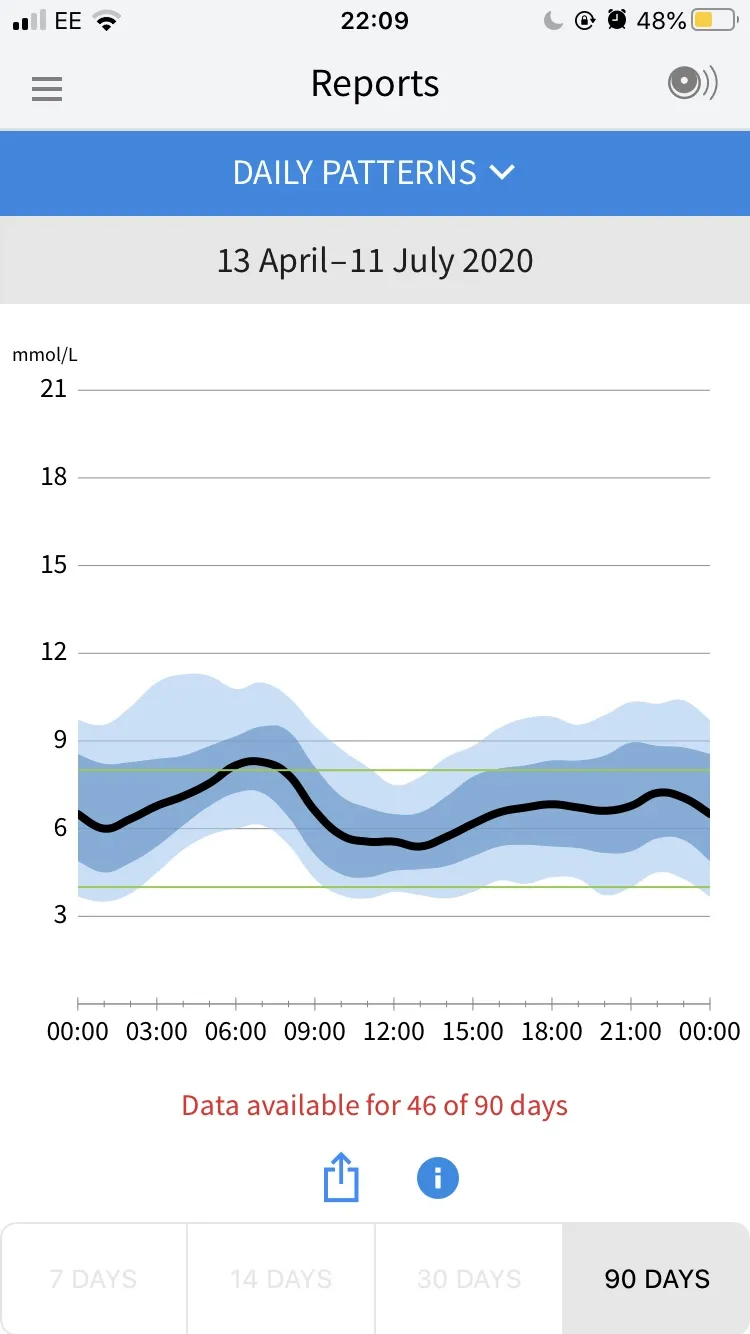
Blood Sugar Monitoring
Regular blood sugar monitoring is a key component of diabetes management during the honeymoon period. Frequent testing allows you to track blood sugar levels and assess how your body responds to insulin, diet, exercise, and other factors. The frequency of blood sugar testing depends on individual needs and the recommendations of your healthcare provider. It may involve testing multiple times a day, especially before meals, after meals, and before bed. The collected data provides insight into how your body responds, enabling you to make necessary adjustments to your insulin dosages, diet, or exercise routine. Utilizing continuous glucose monitors (CGMs) can provide more detailed information on blood sugar trends and fluctuations.
The Role of Education and Support

Education and support play a crucial role in successful diabetes management, particularly during the honeymoon period. Educating yourself about diabetes, its management, and the specific strategies to prolong the honeymoon can empower you to take control of your health. Working with a certified diabetes educator (CDE) or a healthcare team can provide valuable information and support, helping you understand your condition and create a personalized management plan. Joining support groups, either in person or online, can connect you with others who are experiencing similar challenges, providing a sense of community and shared understanding. Learning from the experiences of others can boost your confidence and motivation.
When the Honeymoon Ends
The end of the honeymoon period signifies a gradual decline in the body’s natural insulin production. As the beta cells are progressively damaged by the autoimmune response, the ability to produce insulin diminishes, which leads to rising blood sugar levels. Recognizing the signs of the end of the honeymoon is crucial for effective diabetes management. The transition out of the honeymoon phase can be a challenging time, requiring adjustments to medication, diet, and lifestyle. Working closely with your healthcare provider is vital to manage the transition and maintain good blood sugar control. Understanding this phase helps you adjust and embrace the new diabetes management plan.
Recognizing the Signs
Recognizing the signs that the honeymoon period is ending involves monitoring several factors. You may notice an increase in blood sugar levels, as reflected in your blood glucose readings. Increased thirst and frequent urination, which were initially controlled, might return. You may also find yourself feeling more tired and experiencing other diabetes-related symptoms. Increased insulin needs, such as having to adjust insulin dosages, may indicate a declining beta cell function. Recognizing these signs allows you to work with your healthcare team to make necessary adjustments in your treatment plan. Regular check-ups and open communication with your healthcare provider are essential during this time.
Managing Diabetes Long-Term

Long-term diabetes management requires a comprehensive approach that includes medication, healthy eating, regular physical activity, and regular blood sugar monitoring. It’s also important to have regular check-ups with your healthcare provider and to stay informed about diabetes management. The goal is to maintain healthy blood sugar levels, prevent complications, and live a fulfilling life. This means a lifelong commitment to healthy habits and ongoing medical care. By understanding the specifics of your condition and working in partnership with your healthcare team, you can effectively manage diabetes and prevent health complications.
Conclusion
The diabetes honeymoon period represents a valuable window of opportunity to improve the long-term management and trajectory of the disease. By understanding the characteristics of this period, adopting strategies to prolong it, and effectively managing blood sugar levels, individuals can improve their quality of life and reduce the risk of complications. Early diagnosis, intensive insulin therapy, lifestyle modifications, regular blood sugar monitoring, and access to education and support are key elements in successfully navigating this phase. Remember, the end of the honeymoon doesn’t mean the end of effective diabetes management; with proper care, long-term health and well-being are achievable. Embrace the opportunity to take control of your health, stay informed, and collaborate with your healthcare team for the best possible outcome.
